Abstract
Introduction In sickle cell disease (SCD), hemoglobin S rapidly forms intracellular polymers in the deoxygenated state, resulting in red blood cell sickling, hemolysis, and vaso-occlusion. These changes alter cerebral perfusion and dramatically increase risk for neurocognitive deficits and stroke (Bush et al., 2014; Wang et al., 2021). Voxelotor (Oxbryta®) is an inhibitor of HbS polymerization that has been shown to significantly improve anemia and reduce hemolysis in sickle cell disease. However, it is unknown whether these changes are accompanied by improvements in perfusion and reductions in cerebral metabolic stress. Here we employ two novel optical techniques known as frequency-domain near-infrared spectroscopy (FDNIRS) and diffuse correlation spectroscopy (DCS) to non-invasively monitor regional changes in oxygen extraction fraction (OEF), cerebral blood flow (CBF), and cerebral metabolic rate of oxygen (CMRO2) as markers of cerebral metabolic stress in a pilot cohort of children with SCD beginning voxelotor. Our primary objective was to test the hypothesis that voxelotor decreases CBF, OEF, and CMRO2 from pre-treatment levels. We also explored the relationship between CBF, OEF, and CMRO2 and hemoglobin.
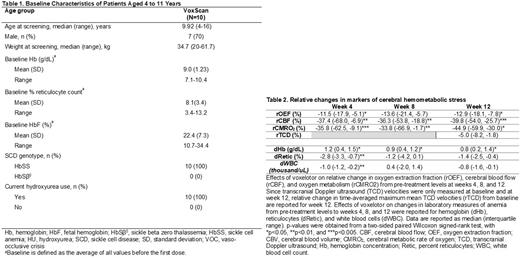
Methods Children ages 4 to 17 years old with SCD (HbSS or HbS-thalassemia) were enrolled at Children's Healthcare of Atlanta. Participants who met study criteria started open label voxelotor at recommended dose. Participants were monitored prior to treatment initiation, as well as at weeks 4, 8, and 12 weeks. At each study visit, laboratory measurements of anemia (CBC, Retic) and FDNIRS/DCS measurements of regional cerebral blood flow, oxygen extraction fraction, and oxygen metabolism were made (Lee et al., 2022). Transcranial Doppler ultrasound (TCD, middle cerebral artery, internal carotid artery, and carotid bifurcations) along with markers of hemolysis (LDH, T.Bili) were performed at weeks 0 and 12. Paired Wilcoxon signed-rank tests were used to test whether all measures were significantly different from pre-treatment levels. Linear mixed-effects regression models with random-intercept at the patient level were used to examine the association of the relative change in each outcome measure (OEF, CBF, and CMRO2) from pre-treatment levels and delta changes in laboratory data. These models were two-level and accounted for repeated measures nested within each patient.
Results Ten of the 12 recruited patients met study criteria. All patients were HbSS on stable dose of hydroxyurea (Table 1). Following initiation of voxelotor, the median (interquartile range, IQR) blood hemoglobin levels increased by 1.2 (0.4, 1.5) g/dL at week 4 (p=0.023); these increases persisted at weeks 8 and 12. Bilirubin was significantly decreased at week 12 (p=0.008), and LDH increased, although the trend was not statistically significant (p=0.24). While TCD velocities were unchanged at week 12, significant decreases in OEF, CBF, and CMRO2 were observed by week 4 (all p < 0.05) that persisted at weeks 8 and 12 (Table 2). Across all time points, relative changes in OEF, CBF, and CMRO2 from pre-treatment levels were inversely associated with changes in hemoglobin (p = 0.0015, 0.071, and 0.020, respectively).
Discussion Non-invasive FDNIRS/DCS was used to successfully measure changes in regional cerebral blood flow and oxygen utilization in response to treatment with voxelotor. Results suggest that voxelotor treatment in children with SCD reduces cerebral metabolic stress by improving oxygen delivery to the tissue. Work is ongoing to validate these measurements with MRI.
Disclosures
Brown:Novo Nordisk: Consultancy; Global Blood Therapeutics: Consultancy, Current Employment, Current equity holder in publicly-traded company, Research Funding; Imara: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Research Funding; Forma Therapeutics: Research Funding. Buckley:Global Blood Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal